The Cayman Islands Mosquito Research & Control Unit
Mosquito control is critically dependent on harnessing local knowledge and skills within communities. Community engagement and mobilization involves working with local residents to improve mosquito control and build resilience against disease outbreaks.

Public Education
Public education is a key component that is used to encourage the reduction and prevention of mosquito habitats on private and public property. MRCU’s education program teaches the public how to recognize, prevent, and suppress mosquito breeding on their property. This is accomplished through the distribution of brochures, fact sheets, newsletters, participation in local events and fairs, presentations to community organizations, newspaper and radio advertising, public service announcements, social media, and contact with MRCU staff in response to service requests. Public education also includes school presentations that teach future adults to be responsible by preventing and/or eliminating mosquito breeding sources.
Mosquito Lifecycle
Mosquitoes (Order Diptera, Family Culicidae) are some of the most adaptable and successful insects on Earth and are found in some extraordinary places. Virtually any natural or man-made collection of water can support mosquito production. They’ve been discovered in mines nearly a mile below the surface, and on mountain peaks at 14,000 feet, and if you know where to look, there is a good possibility that there are mosquitoes breeding in your own backyard. Not every species of mosquito causes problems for people, but many have profoundly negative effects. Mosquitoes can be distinguished easily from other flies by the fact that they have both a long, piercing proboscis and scales on the veins of their wings. Approximately 35 species of mosquitoes are found in the Cayman Islands, with more than 3,000 species known throughout the world. In the Cayman Islands, only a few of these species are important as carriers of disease, but many more are important nuisance species that dramatically affect peoples’ quality of life.

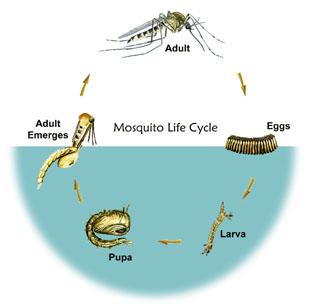
While all mosquitoes need standing water to reproduce, different mosquito species are found in different habitats. Some mosquitoes are considered “floodwater” species that breed in temporary water habitats, while others are considered “permanent water” mosquitoes and breed in water sources that remain for long periods of time. Other species have evolved so specifically that they will only lay their eggs in natural or artificial containers. No matter what their preferred breeding habitat, all mosquitoes undergo the same four-stage life cycle: egg, larva, pupa, and adult, with the larval and pupal stages always being aquatic.

Once the egg hatches, the larval stage begins. The larvae of most mosquito species hang suspended from the water surface because they need air to breath. An air tube, called a siphon, extends from the larva’s posterior to the water surface and acts as a snorkel. Larvae filter feed on aquatic microorganisms near the water’s surface. As a defense mechanism, when alarmed, the larvae can dive deeper into the water by swimming in a characteristic “S” motion, which has earned them the nickname “wigglers” or “wrigglers”. As they feed, larvae outgrow their exterior covering and form a new exoskeleton, casting off the old ones. The stages between these molts are called instars. The larval stage has four instars. The length of the larval stage ranges from 4 to 14 days, varying with species, water temperature, and food availability.
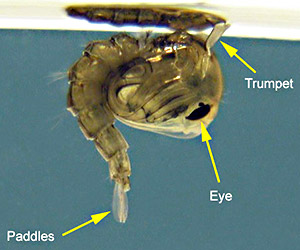
In the pupal stage, no feeding occurs, however the pupa must still breathe air at the water’s surface and is sensitive to light, shadows, and other disturbances. Pupae are also physically active and employ a rolling or tumbling action to escape to deeper water, which is why they are commonly referred to as “tumblers”. The pupal stage lasts from 1 1/2 to 4 days, after which the pupa’s skin splits along the back allowing the newly formed adult to slowly emerge and rest on the surface of the water.

The male adult mosquito will usually emerge first and will linger near the breeding site, waiting for the females. Mating occurs quickly after emergence due to high adult mortality rates. As much as 30% of the adult population can die per day. The females compensate for this high rate by laying large numbers of eggs to assure the continuation of the species. Male mosquitoes will live only 6 or 7 days on average, feeding primarily on plant nectars, and do not take blood meals. Females with an adequate food supply can live up to 5 months or longer, with the average female life span being about 6 weeks. To nourish and develop her eggs, the female usually must take a blood meal in addition to plant nectars. She locates her victims by the carbon dioxide and other trace chemicals exhaled, and the temperature patterns they produce. Mosquitoes are highly sensitive to several chemicals including carbon dioxide, amino acids, and octenol. The average female mosquito’s flight range is between 1 and 10 miles, but some species can travel up to 40 miles before taking a blood meal. After each blood meal, the female will oviposit (lay) her eggs, completing the life cycle. While some species oviposit only once, others may lay eggs several times over the course of their lives.
A Brief Guide to Common Mosquitoes of the Cayman Islands.
Although there are in the region of 36 reported species of mosquitoes found in the Cayman Islands some we see more regularly than others. If you have a mosquito problem and want to report it to the department you may be able to help our investigations by taking a short look at this guide.
Aedes taeniorhynchus
The ‘Black Salt-Marsh mosquito.’ This small black mosquito is by far the most abundant pest mosquito in the Cayman Islands. Most of our operational efforts go into the control of this species. This mosquito breeds mainly in the swamps, the female lays her eggs in the mud and when water levels rise they hatch in large numbers. It is a strong flier and can travel long distances, so large numbers emerging on one part of the island can quickly spread. These mosquitoes can be found year round, but numbers peak in the rainy season. They are active around sunrise and sunset.
Psorphora ciliata and Psorophora columbiae

.
.
.
Culex nigripalpus
This small brown mosquito will breed almost anywhere, but the most saline parts of the swamp, it can be found in natural pools and ponds as well as crab holes and artificial breeding sites like buckets.
.
.
Culex quinquefasciatus

.
.
Aedes aegypti
Aedes aegypti or the ‘Yellow Fever Mosquito’ is a very domesticated mosquito. It is found associated with human habitation breeding in water drums, guttering, buckets and discarded trash. It can be controlled by house and business owners by simply clearing up any water holding containers or making sure that water is not allowed to stand for more than a couple of days in e.g. bird baths, pet water bowls, plant pots, etc. it is a distinctive black and white mosquito that bites mostly in the daytime/late afternoon. This mosquito can carry yellow fever, dengue and chikungunya viruses. It is found widespread across Grand Cayman, but help from the public can help to seriously reduce numbers. Clear up trash and other sources of standing water, including buckets, dog bowls, ornamentals, plant pots and tires. Anything that will hold water when it rains will provide the perfect breeding site for this mosquito
Aedes albopictus

.
.
.
Anopheles
There are a number of Anopheles species to be found in the Cayman Islands. They breed mostly in fresh water and are easily identified when biting as they stand ‘end-up’ unlike other mosquitoes that keep their bodies flat. Anopheles stand with their heads down and are often described as needle like in appearance. Of the Anopheles found in the Cayman Islands one species; Anopheles albimanus can carry the malaria parasite. This mosquito can be identified by the ways it stands as well as its distinctive rear white feet. Anopheles like to bite late into the evening.
*Photo credit for Anopheles albimanus by Audio Visual, LSHTM. Wellcome Images. images@wellcome.ac.uk.
*For other photo credits see images.
Mosquito-Borne Diseases
Mosquitoes cause more human suffering than any other organism — over one million people worldwide die from mosquito-borne diseases every year. Not only can mosquitoes carry diseases that afflict humans, they also transmit several diseases and parasites that dogs and horses are very susceptible to. These include dog heartworm, West Nile virus (WNV) and Eastern equine encephalitis (EEE). In addition, mosquito bites can cause severe skin irritation through an allergic reaction to the mosquito’s saliva – this is what causes the red bump and itching. Mosquito vectored diseases include protozoan diseases, i.e., malaria, filarial diseases such as dog heartworm, and viruses such as dengue, encephalitis and yellow fever. CDC Travelers’ Health provides information on travel to destinations where human-borne diseases might be a problem.
Malaria
Chikungunya
Dog Heartworm
Dengue
Yellow Fever
Eastern Equine Encephalitis
St. Louis Encephalitis
LaCrosse Encephalitis
Western Equine Encephalitis
West Nile Virus
Zika Virus
MALARIA
Malaria is an ancient disease. In all likelihood originating in Africa, it has been described by the Chinese as far back as 2700BC and the Sumerians from 1700 BC. The malaria parasite (plasmodium) is transmitted by female Anopheles mosquitoes. The term malaria is attributed to Horace Walpole in a letter from Italy in 1740 and is derived from the Italian ‘mal-aria” or “bad air” because it was thought to come on the wind from swamps and rivers. Scientists conducted much research on the disease during the 1880s and early 1900s. Approximately 40% of the world’s population is susceptible to malaria, mostly in the tropical and sub-tropical areas of the world. It was by and large eradicated in the temperate area of the world during the 20th century with the advent of DDT and other organochlorine and organophosphate mosquito control insecticides. An elevated standard of living, including the use of air conditioners and window screens, along with public health interventions have largely remanded malaria transmission to tropical areas. Nonetheless, it can still be found in northern Europe.
More than one million deaths and 300 – 500 million cases are still reported annually in the world. It is reported that malaria kills one child every 40 seconds. In the United States malaria affected colonization along the eastern shore and wasn’t effectively controlled until the 1940s when mosquito control organization instituted Anopheles control programs. A resurgence occurred during the 1960s and early 70s in the United States due to returning military personnel from Vietnam. Minor outbreaks of locally-acquired malaria occur sporadically in the United States, but have been quickly controlled by aggressive mosquito control measures. The influx of illegal immigrants in addition to returning tourists may provide for infrequent outbreaks in the future.
Anopheles quadrimaculatus and Anopheles freeborni have been the primary vector of the Plasmodium vivax (protozoa) in the United States (Foote and Cook 1959).
Antimalarial drugs have been available for more than 50 years and recently scientists in Britain and the United States have cracked the code of the malaria parasite genome, a step that may help boost the campaign against the disease. In the meantime, active case detection
Top
CHIKUNGUNYA
Chikungunya virus is a pathogen transmitted by mosquitoes, and has established itself in the Caribbean (approximately 350,000 suspected cases in the Western Hemisphere since December 2013). It has now resulted in 2 cases of locally-transmitted Chikungunya virus in Florida in July of 2014. As of July 22, 2014, 497 travel-related cases have been found in 35 states, Puerto Rico and the U.S. Virgin Islands. The occurrence of locally-transmitted cases causes public health officials fear to its spread and establishment in states bordering the Caribbean. The name “Chikungunya” is attributed to the Kimakonde (a Mozambique dialect) word meaning “that which bends up”, which describes the primary symptom – excruciating joint pain. Although rarely fatal, the symptoms are debilitating and may persist for several weeks. There is no vaccine and primary treatment is limited to pain medication.
The mosquito species that transmit this disease are the Asian Tiger Mosquito (Aedes albopictus) and the Yellow Fever Mosquito (Aedes aegypti). Genetically, it appears that viral strain currently spreading throughout the Americas is more easily transmitted by Ae. aegypti. Both species lay their eggs in containers such as cans, discarded tires and other items that hold water close to human habitation, but Ae. aegypti is more geographically confined to the southeastern United States. Traditional mosquito methods of truck-mounted and aerial sprays are ineffective in controlling these mosquitoes. Removal of water-bearing containers and sanitation are key preventive strategies.
Top
DOG HEARTWORM (DIROFILARIA IMMITIS)
Dog HeartwormDog heartworm (Dirofilaria immitis) can be a life-threatening disease for canines. The disease is caused by a roundworm. Dogs and sometimes other animals such as cats, foxes and raccoons are infected with the worm through the bite of a mosquito carrying the larvae of the worm.
altIt is dependent on both the mammal and the mosquito to fulfill its life cycle. The young worms (called microfilaria) circulate in the blood stream of the dog. These worms must infect a mosquito in order to complete their lifecycle. Mosquitoes become infected when they blood feed on the sick dog. Once inside the mosquito the microfilaria leave the gut of the mosquito and live in the body of the insect, where they develop for 2-3 weeks. After transforming twice in one mosquito the third stage infective larvae move to the mosquito’s mouthparts, where they will be able to infect an animal. When the mosquito blood feeds, the infective larvae are deposited on the surface of the victim’s skin. The larvae enter the skin through the wound caused by the mosquito bite. The worms burrow into the skin where they remain for 3-4 months. If the worms have infected an unsuitable host such as a human, the worms usually die. The disease in dogs and cats cannot be eliminated but it can be controlled or prevented with pills and/or injections. Some risk is present when treating dogs infected with heartworms but death is rare; still prevention is best. Of course good residual mosquito control practices reduce the threat of mosquito transmission. Until the late sixties, the disease was restricted to southern and eastern coastal regions of the United States. Now, however, cases have been reported in all 50 states and in several provinces of Canada.
Arthropod-borne viruses (arboviruses) are the most diverse, numerous and serious diseases transmitted to susceptible vertebrate hosts by mosquitoes and other blood-feeding arthropods. Arboviral encephalitides are primarily zoonotic, being maintained in complex life cycles involving a nonhuman primary vertebrate host and a primary arthropod vector. These cycles usually remain undetected until humans encroach on a natural focus, or the virus escapes this focus via a secondary vector or vertebrate host as the result of some ecologic change. Humans and domestic animals can develop clinical illness but usually are “dead-end” hosts because they do not produce significant viremia, and do not contribute to the transmission cycle. There are several virus agents of encephalitis in the United States: West Nile virus (WN), eastern equine encephalitis (EEE), western equine encephalitis (WEE), St. Louis encephalitis (SLE), La Crosse (LAC) encephalitis, dengue and yellow fever all of which are transmitted by mosquitoes. Another virus, Powassan, is a minor cause of encephalitis in the northern United States, and is transmitted by ticks. A new Powassan-like virus has recently been isolated from deer ticks. Encephalitis is global, in Asia, for example, about 50,000 cases of Japanese encephalitis (JE) are reported annually.
Top
DENGUE
Dengue is a serious arboviral disease of the Americas, Asia and Africa. Although it has a low mortality, dengue has very uncomfortable symptoms and has become more serious, both in frequency and mortality, in recent years. Aedes aegypti and Ae. albopictus are the vectors of dengue. These mosquitoes prefer to lay their eggs in containers close to human habitations and are not well-controlled by standard spraying techniques. The spread of dengue throughout the world can be directly attributed to the proliferation and adaptation of these mosquitoes. Over the last 16 years dengue has become more common, for example; in south Texas 55 cases were reported in 1999 causing one death. More recently, Hawaii recorded 85 cases of dengue during 2001 and the Florida Keys reported over 20 cases in 2010. In 2004 Venezuela has reported more than 11,600 cases classic dengue fever and over 700 cases of DHF. Indonesia dengue outbreak has caused over 600 deaths and more than 54,000 cases. In 1999, Laredo and Nuevo Laredo had an outbreak of almost a 100 cases.
In 2010, Puerto Rico experienced its largest outbreak, with 21,000 cases reported. In 2009, Florida reported the first cases of local dengue transmission in 75 years, within Old Town, Key West. A serosurvey of residents suggested an infection rate of 5%, indicating serious risk of transmission. Despite thorough control efforts carried out by the county and state in early 2010, by the end of 2010, Florida had reported an additional 65 locally acquired dengue cases. All the cases were in Key West, except two cases in two more northerly counties.
Top
YELLOW FEVER
Yellow fever, which has a 400-year history, at present occurs only in tropical areas of Africa and the Americas. It has both an urban and jungle cycle. It is a rare illness of travelers anymore because most countries have regulations and requirements for yellow fever vaccination that must be met prior to entering the country (http://www.cdc.gov/ncidod/dvbid/yellowfever/index.htm). Every year about 200,000 cases occur with 30,000 deaths in 33 countries. It does not occur in Asia. Over the past decade it has become more prevalent. In 2002 one fatal yellow fever death occurred in the United States in an unvaccinated traveler returning from a fishing trip to the Amazon. In May 2003, 178 cases and 27 deaths caused by yellow fever were reported in southern Sudan. In the Americas 226 cases of jungle yellow fever have been reported with 99 deaths (ProMed 12-22-03).
Top
EASTERN EQUINE ENCEPHALITIS (EE)
Eastern Equine Encephalitis (EEE) is spread to horses and humans by infected mosquitoes. It is among the most serious of a group of mosquito-borne arboviruses that can affect the central nervous system and cause severe complications and even death. EEE is found in freshwater hardwood swampland in the Atlantic and Gulf Coast states in the eastern part of North America, Central and South America, and the Caribbean. It has a complex life cycle involving birds and a specific type of mosquitoes including several Culex species andCuliseta melanura. These mosquitoes feed on infected birds and become carriers of the disease and then feed on humans, horses and other mammals. EEE cannot be transmitted from humans or other mammals because the viremia presented in the disease is not sufficient to further transmission. Thus, humans and other animals are known as “dead-end hosts.” Symptoms may range from none at all to a mild flu-like illness with fever, headache, and sore throat. More serious infections of the central nervous system lead to a sudden fever and severe headache followed quickly by seizures and coma. About half of these patients die from the disease. Of those who survive, many suffer permanent brain damage and require lifetime institutional care. There is no specific treatment. A vaccine is available for horses, but not humans.
Top
ST. LOUIS ENCEPHALITIS (SLE)
St. Louis Encephalitis (SLE) is transmitted from birds to man and other mammals by infected mosquitoes (mainly some Culex species). SLE is found throughout the United States, but most often along the Gulf of Mexico, especially Florida. Major SLE epidemics occurred in Florida in 1959, 1961, 1962, 1977, and 1990. The elderly and very young are more susceptible than those between 20 and 50. During the period 1964-1998 [35 years] a total of 4478 confirmed cases of SLE were recorded in the United States Symptoms are similar to those seen in EEE and like EEE, there is no vaccine. Mississippi’s first case of St. Louis Encephalitis since 1994 was confirmed in June 2003. Previously the last outbreak of SLE in Mississippi was in 1975 with over 300 reported cases. It was the first confirmed mosquito-borne virus in the United States in 2003. It turned up in October 2003 in California Riverside County in sentinel chickens. The last [SLE] human case in California occurred in 1997. In Louisiana in 2003 there was a fatal St Louis Encephalitis case previously listed as a West Nile caused death.
Top
LACROSSE ENCEPHALITIS (LAC)
LaCrosse encephalitis (LAC) is much less widespread than EEE or SLE, but approximately 90 cases occur per year occurs in all 13 states east of the Mississippi, particularly in the Appalachian region. It was reported first in 1963 in LaCrosse, Wisconsin and the vector is thought to be a specific type of woodland mosquito (Aedes triseriatus) called the tree-hole mosquito, with small mammals the usual warm-blooded host. Infrequent fatalities occur in children younger than 16. It is not transmissible from human to human. There is no vaccine for LaCrosse encephalitis.
Top
WESTERN EQUINE ENCEPHALITIS (WEE)
Western Equine Encephalitis (WEE) was first recognized in 1930 in a horse in California. It is found west of the Mississippi including parts of Canada and Mexico. The primary vector is Culex tarsalisand birds are the most important vertebrate hosts with small mammals playing a minor role. Unlike LAC it is nonspecific in humans and since 1964 fewer than 1000 cases have been reported As with EEE a vaccine is available for horses against WEE but not for humans. In Arizona 3 counties have been found with sentinel chicken flocks seroconverting to WEE.
Top
WEST NILE VIRUS (WNV)
West Nile virus (WNV) emerged from its origins in 1937 in Africa (Uganda) into Europe, the Middle East, west and central Asia and associated islands. It is a Flavivirus (family Flaviviridae) with more than 70 identified viruses. Serologically, it is a Japanese encephalitis virus antigenic complex similar to St. Louis, Japanese and Murray Valley encephalitis viruses. Similar to other encephalitises, it is cycled between birds and mosquitoes and transmitted to mammals (including horses) and man by infected mosquitoes. WNV might be described in one of four illnesses: West Nile Fever might be the least severe in characterized by fever, headach, tireness and aches or a rash. Sort of like the “flu”. This might last a few days or several weeks. At least 63% of patients report symptoms lasting over 30 days, with the median being 60 days. The other types are grouped as “neuroinvasive disease” which affects the nervous system; West Nile encephalitis which affects the brain and West Nile meningitis (meningoencephalitis) which is an inflammation of the brain and membrane around it. (CDC)
It first appeared in North America in 1999 in New York (Cornell Environmental Risk Analysis Program) with 62 confirmed cases and 7 human deaths. Nine horses died in New York in 1999. In 2001, 66 human cases (10 deaths) were reported in 10 states. It occurred in birds or horses in 27 states and Washington D.C., Canada and the Caribbean. There were 733 horse cases in 2001 with Florida reporting 66% of the cases; approximately 33% were fatal. In 2001 more than 1.4 million mosquitoes were tested for WNV. In the United States (2004) over 43 species of mosquitoes have tested positive for WNV transmission, the Culex pipiens group seems the most common species associated with infecting people and horses. Currently, 65 mosquito and 300 bird species have tested positive in the United States for this virus.
During 2002, the number of areas reporting WNV grew to 44 states and 5 Canadian provinces. The only states not reporting WNV were Alaska, Arizona, Hawaii, Nevada, Oregon and Utah that year. Intrauterine transmission (CDC MMWR) and laboratory infections (CDC MMWR) were reported for the first time. In all over 3800 human cases with 232 fatalities in 39 states and Washington DC were recorded. More than 24,350 horse cases of WNV were confirmed or reported in 2002. There is a vaccine for horses. Even alligators (CDC-EID) were found infected in Georgia.
The first confirmed 2003 WNV infection was in South Carolina on July 7th, 2003. South Dakota confirmed a WNV infection in a dog. The final CDC report list 9858 cases. Nebraska had 1942, Colorado 2947 and Idaho only one (CDC) . In Florida there were 94 human cases with most occuring in the panhandle. Bay county, FL reported 14 cases and one death. Of the more than 9858 cases, 6829 were West Nile Fever ( the milder form), 2863 were neuroinvasive (the more severe form) and 166 clinically unspecified. There were over 4200 positive dead birds reported in 39 states and 4500 plus infections in horses in 40 states with more than 425 of these in Colorado. West Nile was reported in 1377 sentinel chicken flocks from 15 states. In Florida 1173 seroconversions to WNV were reported from 34 counties. More than 1950 positive mosquito pools were reported from 32 states and New York City.
In Canada (01-12-04) WNV was been confirmed in 9 Provinces. At least 10 human deaths and more than 1220 cases have been confirmed. Canada reported over 445 presumed or confirmed horse cases in 6 Provinces with over 180 in Alberta Province. Five Provinces have reported positive mosquito pools (>575) with over 290 from Manitoba. Canada confirmed over 1600 positive dead birds from 12000 tests.
Mexico (December 2003) has tested over 590 citizens in 25 states. Six have tested positive with three with the more severe form of WNV. Mexico horse data shows 2475 had positive WN returns in 29 states. Of more than 18000 birds tested 117 were positive. The Pan American Health Organization (PAHO).
Arizona and New Mexico reported the first human cases of WNV on May 26, 2004 and a week later confirmed a total of 7 cases. South Dakota reported it’s first case on June 8, 2004. In 2003 South Dakota had 14 deaths and over human cases reported. Wyoming and Florida (http://www.heraldtribune.com/) has joined the list recently. Alabama, Arizona, Texas and Virginia have reported WN V infections in horses. WNV seroconversions have been reported in 64 sentinel chicken flocks from 4 states (Arizona, California, Florida, and Louisiana), and 58 WNV-positive mosquito pools have been reported from 6 states (Arizona, California, Illinois, Indiana, Louisiana, and Pennsylvania).
As of 2014, there have been 36,437 cases of WNV reported to CDC. Of these, 15,774 have resulted in meningitis/encephalitis and 1538 were fatal. CDC estimates that there have been at least 1.5 million infections (82% are asymptomatic) and over 350,000 cases of West Nile Fever, but the disease is grossly under reported due to its similarity to other viral infections.
Canada’s 1st dead bird (a blue jay) from West Nile virus in 2004 was confirmed in Ontario in May 2004. West Nile virus was confirmed in 2 birds in Puerto Rico near the former US Roosevelt Roads Navy Base (southeastern Puerto Rico).
Britain’s Health Protection Agency has started its annual surveillance program for possible human cases of West Nile virus infection. The program, which has been used for the last three years, operates during the summer, when there is West Nile virus activity in other countries. The UK has had no reported WNV, but are developing a West Nile Virus Contingency Plan.
Top
ZIKA VIRUS
Zika virus has emerged from its origins in central Africa and has rapidly spread to the South Pacific and western hemisphere. A Flavivirus related to West Nile, Yellow Fever, St Louis and the equine encephalitides, Zika was first discovered in macaque monkeys in 1947 in the Zika Forest region of Uganda. Since its discovery in 2014 off the coast of South America, Zika cases have been found in 35 countries in the Americas.
As of 28 April, 2016, there have been 426 reported cases of Zika virus due to travel to endemic areas. However, local transmission within the continental United States has, as yet, not been reported. In US Territories in the Caribbean, a total of 599 cases have been reported, with 596 being locally acquired, primarily in Puerto Rico and the US Virgin Islands.
Although in rare cases Zika can be spread through sexual contact with an infected person, it is usually transmitted through the bit of an infected Aedes agypti or Aedes albopictus mosquito. The illness is usually quite mild, with fever, rash, conjunctivitis and joint pain lasting a few days to several weeks or months. Often patients are not sick enough to seek medical treatment so a great many cases are not reported. It is thought that one attack confers immunity. However, cases of microcephaly, a congenital defect of cranium and brain size resulting in profound neurological defects in newborns usually resulting in death have been been positively identified as being caused by Zika infection. An autoimmune condition called Guillain-Barré syndrome, causing damage to nerve cells resulting in muscle weakness and, on occasion, paralysis and death has been linked to Zika infection.
The mosquito vectors of Zika virus are peridomestic, preferring to lay their eggs above the waterline of containers, treeholes, creases in tarpaulins and other vessels that may contain water. Aedes aegypti, in particular, will lay eggs in a series of containers after feeding. Both Aedes agypti and Aedes albopictus will feed day or night when a potential host comes within their limited flight ranges. Aedes agypti has more of a tendency to enter and stay within houses if conditions are proper. This species is exceedingly skittish, often leaving its host prior to taking a full blood meal when the host moves. Both mosquitoes also seem to prefer feeding on the host’s lower extremities.
Traditional outdoor ULV sprays are ineffective against Aedes agypti, it being difficult to obtain contact with the spray droplets in flight due to its cryptic habits. Some success with ULV sprays has been obtained against Aedes albopictus in urban areas, while suburban areas remain refractory. The primary means of controlling both species is to eliminate their oviposition habitats by removing water bearing containers or emptying them and scrubbing the insides to remove eggs deposited above the waterline. Personal protective measures such as application of EPA-registered repellents and wearing of long-sleeved shirts and long pants are also effective measures.
When traveling to areas endemic for Zika in the Caribbean, it is also recommended to stay in hotels with air conditioning and window and door screens to keep mosquitoes outside. If available, it is advised to sleep under mosquito bed nets.